Obstructive Sleep Apnea and Treatment Options
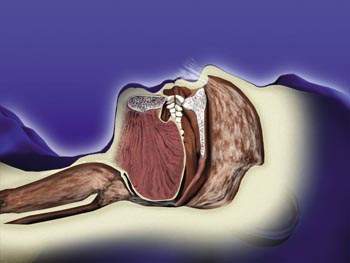
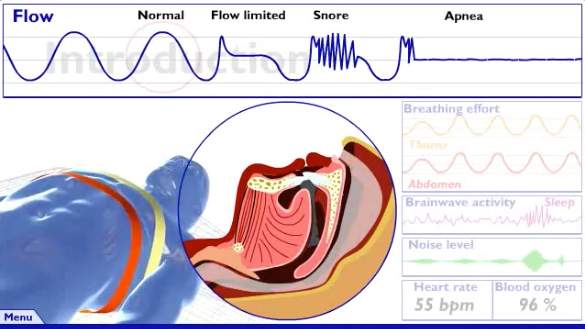
Obstructive sleep apnea (OSA) is characterized by repetitive episodes of complete or partial obstructions of the upper airway throughout the night. These respiratory obstructions can profoundly affect sleep and result in many awakenings through the course of a given night. OSA can lead to systemic effects on the entire body. Moderate to severe sleep apnea has been shown to increase the risks for stroke, cardiac arrhythmias, hypertension and type II diabetes. We determine the apnea hypopnea index (AHI) to quantify the severity of obstructive sleep apnea. AHI represents the average number of respiratory events per hour. We further characterize the obstructions as a partial (reduced airflow during sleep), or a complete respiratory airway closure. These events are referred to as hypopneas and apneas (no airflow) respectively. When evaluating sleep apnea, we start with a focused history and perform a physical exam that includes an assessment of the airway. Any patient with a high degree of suspicion for sleep disordered breathing will require testing to provide objective data confirming a diagnosis. This can be done with either an in-lab polysomnogram or a home sleep apnea test (HSAT). Both tests have a high degree of sensitivity and specificity for detecting sleep apnea. Polysomnography is a more comprehensive test which also records EEG (electroencephalogram), EOG (electrooculogram), EMG (electromyogram) and EKG (electrocardiogram). All polysomnography tests are performed within our sleep lab. EEG are electrical impulses produced by the brain which we can use to score one of four different sleep stages. The best therapy for OSA is positive airway pressure (PAP therapy). Positive airway pressure delivers a constant flow of air through an open circuit device (CPAP machine).
The result is a pressurized environment inside the upper airway. This positive pressure displaces soft tissue out of the way so you can breathe. The soft palate and anatomical structures located along the lateral aspects of the upper airway are often the main sites responsible for airway occlusion while you sleep. Auto-CPAP can overcome collapsing soft tissue by delivering an increasing range of pressures necessary to keep you breathing. Auto-CPAP devices can “sense” when your airway is open, and lock in at that pressure required to treat your obstructive sleep apnea. There are a wide spectrum of PAP devices including: Bi-level PAP (adjusts to a lower pressure as you exhale for more comfort), auto-CPAP and ASV (adaptive servo ventilation). These devices can be adjusted or “tweaked” by a sleep specialist for your comfort. Some of the features we commonly adjust include: humidity setting, smart sensing (automatically turns on when you put on your mask) and ramp time (gives you a pre-set time to fall asleep before auto-adjusting your pressure up). Mask discomfort is a common reason for poor patient CPAP compliance. We now have many different types of mask interfaces to choose from. A mask should be relatively loose fitting and be able fit your facial contour comfortably. A small population of patients will be unable to tolerate CPAP even after an initial adjustment period. For patients who fail PAP therapy, we can provide a dental referral for oral devices as an alternative to PAP therapy. For an oral device, (mandibular advancement device) a certified dentist will use equipment to design and fit a device specific to your teeth, jaw line and bite points. The oral appliance can be further adjusted (titrated) to overcome snoring or other symptoms related sleep disordered breathing.
CENTRAL SLEEP APNEA
In contrast to obstructive sleep apnea, central sleep apnea (CSA) is the inability of the brain to effectively control breathing while asleep. This condition results in pauses in respiration and is frequently seen along with obstructive sleep apnea. Similar to OSA, central sleep apnea can have a deleterious effect on the heart and lungs and it can lead to dangerously low oxygen saturations levels while sleeping. The cause of central sleep apnea is diverse and often requires extensive work up by a sleep medicine specialist in order to identify the underlying root cause.



